NCATS Director of the Division of Clinical Innovation
Mike's Blog
Planting Trees…
By Michael G. Kurilla M.D., Ph.D.
June 30, 2025
Advice from the Daily Stoic.
In a past geological era (during my college days), I had the opportunity to drive across the country (multiple times). At the time, there were no ATMs, cell phones, or GPS. I made the trek with only a big wad of cash and a Rand McNally map. When my son was of a comparable age, I would comment to him that my generation didn’t have cell phones, computers, or video games growing up, so my generation was forced to invent all that stuff! What is most interesting about this is that we measure progress by our technology, specifically our technological gadgetry. And with all that gadgetry, we tend to view technological advance largely as some combination of faster, better, or cheaper. Also, we prefer technological improvements that offer the least operational or administrative change in our routines. This most easily results in a ‘bolt-on’ mentality where we simply add new technology into our mix without much thought to changing workflows or organizational structures, as well as health care delivery arrangements. But if we are to truly realize the full impact of advancing technology on medicine, we need to think beyond mere gadgetry and consider reimagining how we conceptualize health and how we organize and deliver health care overall including personnel as well as infrastructure. Instead of merely ‘faster, better, or cheaper,’ we need to add ‘different.’
Advancing technology should not only change what we can do, but also ‘how’ we undertake addressing current issues. In addition, advancing technology allows us to ask questions never previously even contemplated. Over the past year, there have been numerous suggestions for NIH reorganization. While I have no enlightened opinions to offer on any of the specific proposals, I do feel that the current NIH structure may not be optimal for truly 21st century scientific and medical research.
As an example, consider Parkinson’s disease; clearly a neurological disorder with a long history of support from NINDS. However, some of the more recent intriguing research findings have come from outside the CNS. The gut-brain axis with heavy involvement of our microbiome has been receiving much attention in the last ten years, including Parkinson’s disease with an emerging consensus that microbiome changes are not simply a consequence of disease progression or medication use. With regards to Parkinson’s diagnostics, a most fascinating piece of work appeared recently utilizing cerumen, AKA earwax and testing for specific volatile organic compounds (VOCs). This follows on the report of a human being capable of ‘smelling’ Parkinson’s disease six years prior to diagnosis (this is also an great example of a clinical observation turned into useful science). Earwax turns out to be an excellent matrix for capturing VOCs which are also released from the skin but easily vaporized away (one more ‘omics to integrate – volatilomics!). In addition, Parkinson’s is not the first disease to sample earwax, as Meniere’s disease has also been diagnosed this way and most recently, even cancer. A recent CTSA publication reported a machine learning algorithm that can diagnose Parkinson’s disease by voice patterns from smartphone recordings. And this is not a unique one-off, as a company in Canada has published results of voice patterns predicting hypertension and Type 2 diabetes. Finally, retinal scans which appear to be informative for diverse medical conditions such as heart disease or dementia has also tried its hand at Parkinson’s disease diagnosis.
So, in addition to NINDS, we may need to add NIDDK, NIAID, NEI, and NIDCD (whose budget is smaller than the CTSA Program) to comprehensively address Parkinson’s disease, and that’s with just our currently available science. And more than likely, this type of scenario is not limited to Parkinson’s disease but represents an emerging appreciation that while our conceptualization of disease originates at the cellular and organ level, manifestations of disease are systemic in nature with impacts on physiologic processes unrelated to etiology. Medicine has always recognized this concept, but advancing technology has now afforded the opportunity for potential game changing exploitation that nearly borders on magic.
Now try to imagine if the above were to apply not just to Parkinson’s disease, but to the vast majority of medical issues. Having an annual checkup could go something like this: Before the checkup, a stool sample is submitted. At the health care facility, a retinal scan and earwax specimen are obtained. Following that, a history and review of systems is obtained by a professional trained to ask specific questions and elicit information while an AI analyzes your voice pattern. During this time, the results of your stool sample analysis (both microbiome constituents as well as metabolites), retinal scan, and your earwax volatilomics analysis (AKA cerumenogram) have been integrated looking for confirmation from your voice pattern assessed against your genome sequence (which was obtained at birth and is part of your EHR) to render either a clean bill of health with some targeted lifestyle recommendations or a follow-up appointment with a physician for any identified or ongoing medical concerns. And you’ll likely have an AI avatar on your smartphone that will receive all the data generated and be able to discuss the visit with you long after the appointment.
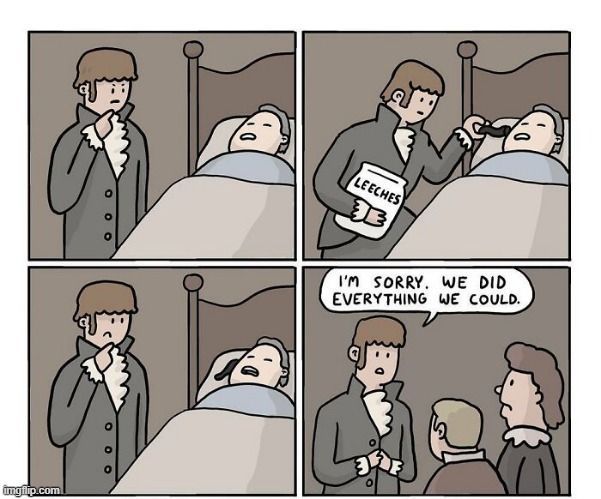
Sounds like science fiction? Sure. But then everything you’re doing right now would have sounded like science fiction (or magic) to this guy:
Of course, there’s lots of work to do, at least a generation’s worth (I’m looking at K scholars and T trainees). Critically, innovative translational pathways are needed for evaluating the suitability for integration of the analyses described above into routine clinical practice similar to blood chemistry. The CTSAs are uniquely situated within our vast, overwhelming, and balkanized academic medical research enterprise to not only develop and validate this emerging science, but to also translate these disparate elements into something truly revolutionary, rather than merely evolutionary and initiate what will someday be regarded as 21st century medicine!
The future is not something we enter. The future is something we create.
Leonard Sweet




