Hub Spotlight: Boston University Clinical and Translational Science Institute
CCOS is pleased to continue our series of hub highlights, celebrating innovative contributions to clinical and translational science across the CTSA Program. Today, we spotlight the Boston University Clinical and Translational Science Institute, a leader in advancing translational research, fostering teamwork, and driving meaningful health impact through cutting-edge evaluation and improvement models.
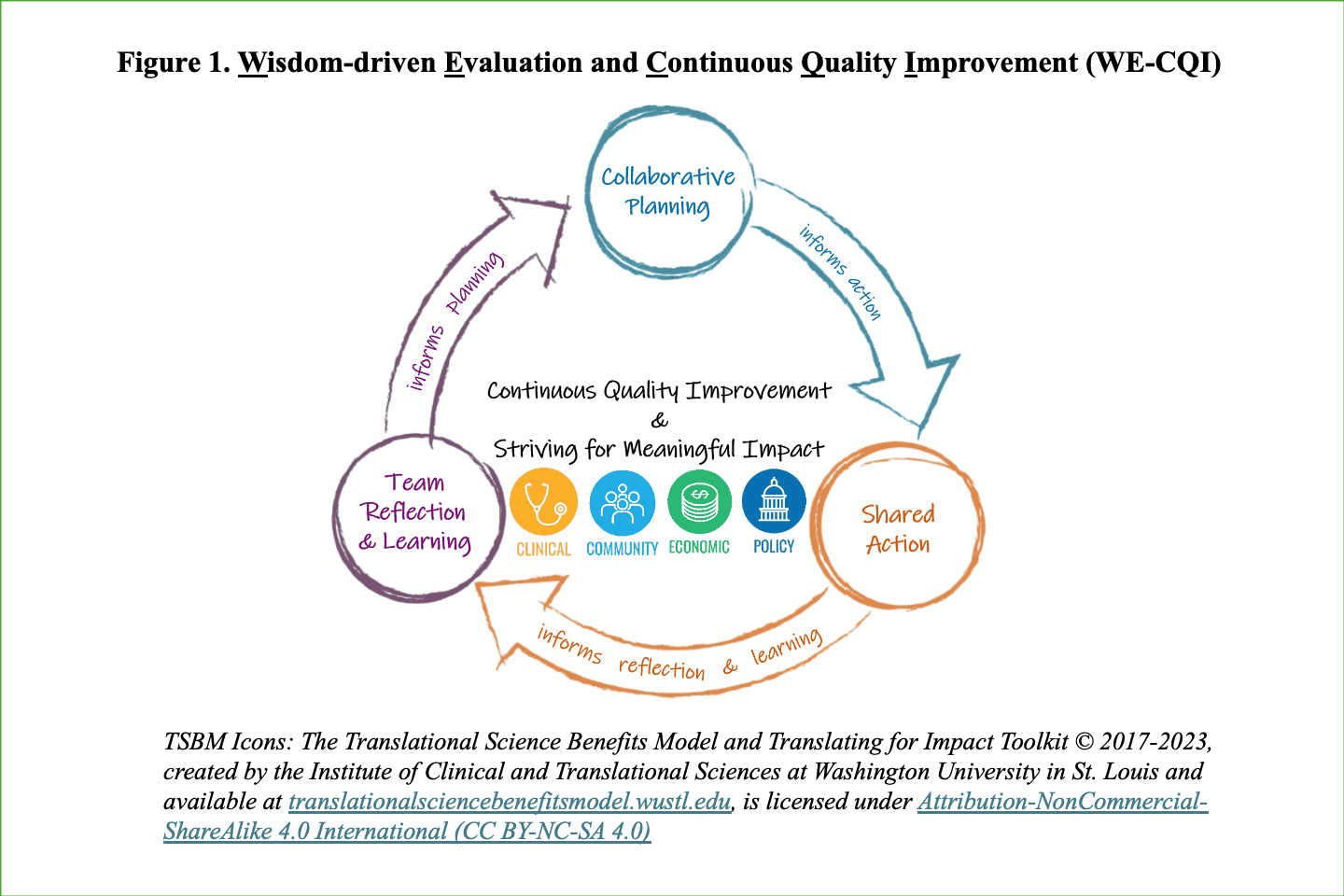
Boston University’s Clinical and Translational Science Institute (BU CTSI) has been a driving force in transforming biomedical research into real-world health solutions since its inception in 2008. With a mission rooted in innovation and collaboration, BU CTSI has consistently pushed the boundaries of what academic research can achieve for patients, communities, and society at large. Over the years, the institute has secured more than $113 million in funding, catalyzing a wide range of initiatives from policy-shaping studies and patents to workforce development and clinical advancements. Recently, BU CTSI published its approach to evaluating and improving its impact: the Wisdom-Driven Evaluation and Continuous Quality Improvement (WE-CQI) model. This framework represents a significant evolution in how translational science is measured and enhanced, not just at BU but across the broader Clinical and Translational Science Award (CTSA) Program network.
At the heart of this transformation is the Translational Science Benefits Model (TSBM), a framework developed by Washington University in St. Louis to address a longstanding challenge in clinical and translational research: how to systematically document and evaluate the broader health and societal impacts of scientific work. Traditionally, research evaluation focuses on outputs such as publications or grant funding. While important, these metrics often fail to capture the true benefits of research for patients, communities, and policy. The TSBM, created by leaders in translational science at Washington University in St. Louis and widely adopted across the CTSA program, provides a structured way to assess impact in four key domains: clinical and medical benefits, community and public health benefits, economic benefits, and policy and legislative benefits. This framework has given CTSA programs a common language for demonstrating how research is translated into the surrounding world.
As the field of translational science has evolved, it became clear that simply measuring impact was not enough. CTSA programs, funded by the NIH, are also required to implement continuous quality improvement (CQI) processes to ensure that their activities are not only effective but are constantly evolving to meet new challenges. Traditional CQI models, such as the Plan-Do-Study-Act cycle, have proven valuable for process improvement but often fall short in the complex, team-based environments that characterize translational science. There was a clear need for a framework that could integrate CQI with impact evaluation in a way that was collaborative, adaptive, and meaningful.
BU CTSI responded to this need by developing the WE-CQI model, which weaves together the strengths of the TSBM, established CQI methodologies, and the principles of team science. Unlike traditional CQI frameworks, the WE-CQI model explicitly incorporates team science principles, encouraging shared leadership and responsibility for evaluation and improvement. The model unfolds in three interconnected phases: collaborative planning, shared action, and team reflection and learning. This structure ensures that evaluation is not a one-time event but an ongoing, collective, and iterative process. Flexibility is a hallmark of the WE-CQI model, allowing teams to adapt their strategies as needs evolve and ensuring that improvements are directly linked to meaningful clinical, community, economic, and policy outcomes.
One of the key innovations of the WE-CQI model is its emphasis on co-creation. All team members are invited to participate in developing evaluation strategies, sharing responsibility for implementing improvements, and engaging in regular reflection and learning to adapt and optimize outcomes. By aligning CQI activities with the TSBM, the model guarantees that the goal remains focused on maximizing real-world impact.
To illustrate the practical application and effectiveness of the WE-CQI model, BU CTSI applied it to its Regenerative Medicine Training Program (RMTP). This initiative prepares scientists for careers in cutting-edge medical research and serves as a living laboratory for the new evaluation framework. The evaluation team employed a mixed-methods approach, combining interviews, document analysis, bibliometric and policy analysis, and surveys to assess the program’s impact from 2015 to 2023.
The results of this case study were compelling. Clinically, 91% of RMTP graduates remain in regenerative medicine research, contributing to the development of new diagnostic and therapeutic procedures. In terms of community impact, graduates are actively translating research into science-based health education for public and community audiences. The program has also generated significant economic benefits, including new patents and industry partnerships that advance cost-effective treatments for organ failure and infectious diseases. On the policy front, RMTP activities have influenced formal quality assurance standards for various health study approaches and treatments.
The WE-CQI model also made several improvements within the RMTP. For example, in response to trainee feedback regarding a lack of community, the program introduced annual luncheons and networking events, which improved peer connections and fostered a stronger sense of belonging. When trainees requested more formal feedback on professional development, the program implemented annual performance reviews and individualized career development plans, providing structured guidance and support for a variety of career pathways.
These changes, guided by the WE-CQI model, were directly linked to improved outcomes and greater impact across all TSBM domains. The model’s emphasis on shared responsibility and continuous learning created an environment where meaningful improvements could be made and sustained.
As public health challenges become increasingly complex, the need to accelerate the translation of research into practice has never been more urgent. CTSA programs are uniquely positioned to bridge this gap, but only if they can effectively evaluate and improve their work. The WE-CQI model offers a roadmap for making evaluation more collaborative, adaptive, and impactful. By sharing their approach and findings, BU CTSI is not only advancing its own mission but also providing a valuable resource for the entire CTSA community. The WE-CQI model stands as a testament to the power of team science, continuous improvement, and a focus on real-world impact.
Check out the full publication to learn more about BU CTSI's work on the WE-CQI model.




